May-Thurner Syndrome & Venous stenting
What is May-Thurner Syndrome?
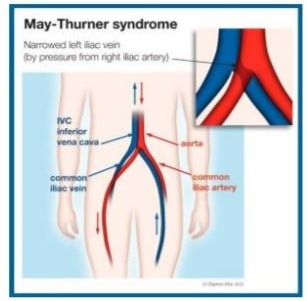
May-Thurner Syndrome is an anatomical abnormality in which the Left Iliac Vein is compressed by the Right Iliac Artery.
Why does May-Thurner Syndrome Matter?
Veins carry blood at much lower pressures than arteries. With the Right Iliac Artery so close, the Left Iliac Vein can be easily obstructed. Even partial obstructions can cause issues. Partial obstructions of the Left Iliac Vein increase the risk of clot formation, particularly for patients who are immobilized (Post-operative, long plane flights, casts).
Treatment for May-Thurner Syndrome
Most May-Thurner patients are asymptomatic and neither diagnosed nor treated. If a patient develops a deep venous thrombosis, they may be referred to a vascular surgeon for further evaluation, which is usually when May-Thurner is diagnosed. Sometimes it is found when evaluating a patient for chronic LEFT leg swelling.
Deep Venous Thrombosis Treatment in May-Thurner Syndrome
A deep venous thrombosis or DVT is a blood clot in the venous system. DVTs can be much more serious in May-Thurner patients, as they are larger, cause more swelling, and may be more likely to cause Pulmonary Embolism. In addition to hospitalization and anticoagulation treatment with Heparin (A blood thinner), these patients often require a stent to be placed in their Left Iliac Vein. The reason they eveloped a DVT was due in large part to their unique anatomy. The stent helps keep the vein open and prevents the formation of future DVTs. Sometimes a patient receiving a stent will be put on an anti-platelet medication like Plavix for three months, and often is maintained on baby aspirin (81mg) for life. Lifetime followup of the stent with yearly ultrasound is also recommended to make sure the vein is not narrowing down again for any reason.
Go Back May-Thurner Syndrome is an anatomical abnormality in which the Left Iliac Vein is compressed by the Right Iliac Artery.
Why does May-Thurner Syndrome Matter?
Veins carry blood at much lower pressures than arteries. With the Right Iliac Artery so close, the Left Iliac Vein can be easily obstructed. Even partial obstructions can cause issues. Partial obstructions of the Left Iliac Vein increase the risk of clot formation, particularly for patients who are immobilized (Post-operative, long plane flights, casts).
Treatment for May-Thurner Syndrome
Most May-Thurner patients are asymptomatic and neither diagnosed nor treated. If a patient develops a deep venous thrombosis, they may be referred to a vascular surgeon for further evaluation, which is usually when May-Thurner is diagnosed. Sometimes it is found when evaluating a patient for chronic LEFT leg swelling.
Deep Venous Thrombosis Treatment in May-Thurner Syndrome
A deep venous thrombosis or DVT is a blood clot in the venous system. DVTs can be much more serious in May-Thurner patients, as they are larger, cause more swelling, and may be more likely to cause Pulmonary Embolism. In addition to hospitalization and anticoagulation treatment with Heparin (A blood thinner), these patients often require a stent to be placed in their Left Iliac Vein. The reason they eveloped a DVT was due in large part to their unique anatomy. The stent helps keep the vein open and prevents the formation of future DVTs. Sometimes a patient receiving a stent will be put on an anti-platelet medication like Plavix for three months, and often is maintained on baby aspirin (81mg) for life. Lifetime followup of the stent with yearly ultrasound is also recommended to make sure the vein is not narrowing down again for any reason.