Common Myths about Varicose Veins
Varicose veins are quite common and often lead to pain, embarrassment and possibly further health issues. According to the American Society for Vascular Surgery, 20-25 million Americans have varicose veins.
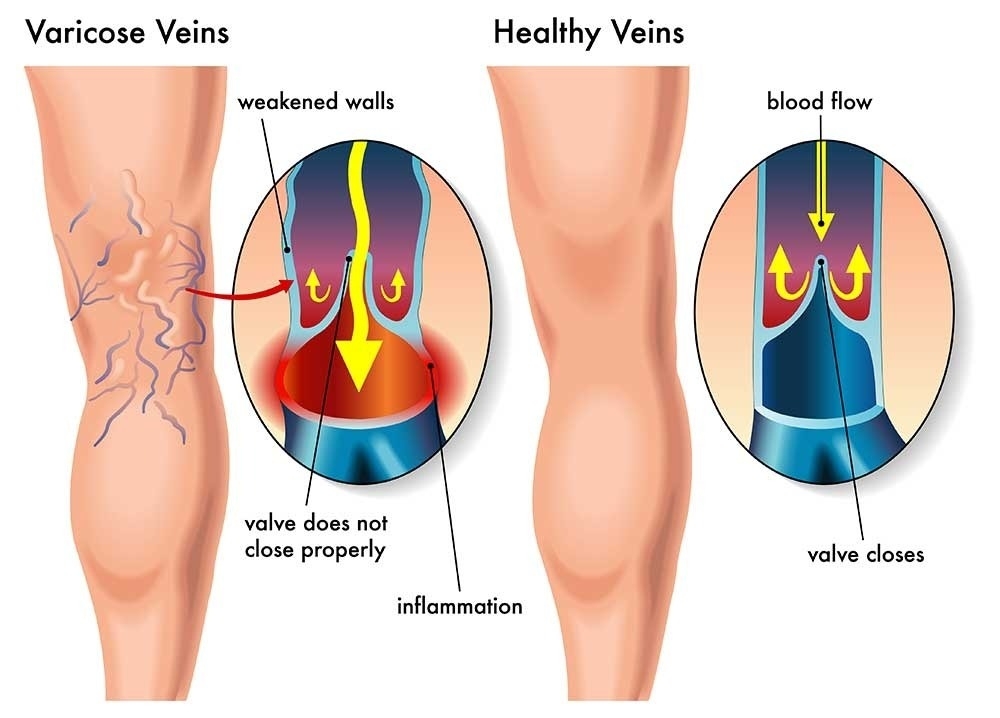
Varicose veins often present as blue, rope-like vessels under the skin usually in the legs and feet. Varicose veins are often painful and unsightly. Usually caused by reflux or valves not working properly, the reversal of blood flow and venous stasis (slow blood flow or pooling) may result in leg swelling (Edema), skin changes and in more severe cases, venous ulcers, if left untreated.
Given the prevalence of varicose veins, many myths continue to surround them. The physicians at the Vascular Institute of the Rockies, the largest vascular group in the Rocky Mountain region, will debunk some of these top myths.
Varicose veins are common and often present as rope-like blue vessels typically in the legs or feet. Varicose veins are oftentimes painful presenting with symptoms such as heaviness/fatigue in legs, leg swelling, restless leg syndrome, leg cramping while sleeping, pain, itching and burning. If left untreated, varicose veins may results in leg swelling, skin changes or venous ulcers in more severe cases.
If you have questions or concerns about varicose veins or your lifestyle is being negatively impacted by the pain and discomfort of varicose veins, talk to your doctor today. A primary care physician can recommend you to a vascular specialist that can quickly and easily treat your varicose veins today.
If you’d like more information about varicose veins, please refer to your FAQ or watch our video. Feel free to reach out to us if you’d like to speak directly to a vascular specialist.
Go Back Varicose veins often present as blue, rope-like vessels under the skin usually in the legs and feet. Varicose veins are often painful and unsightly. Usually caused by reflux or valves not working properly, the reversal of blood flow and venous stasis (slow blood flow or pooling) may result in leg swelling (Edema), skin changes and in more severe cases, venous ulcers, if left untreated.
Given the prevalence of varicose veins, many myths continue to surround them. The physicians at the Vascular Institute of the Rockies, the largest vascular group in the Rocky Mountain region, will debunk some of these top myths.
Myth #1: Varicose veins are only cosmetic.
While varicose veins are certainly visible on your legs, they can significantly impact your health and well-being. People may experience heaviness/fatigue in their legs, leg swelling, Restless Leg Syndrome, leg cramping while sleeping, color changes in skin, pain, itching, burning, and an increased risk of blood clots.Myth #2: Only women get varicose veins.
While it is more common for women to have varicose veins, men certainly have them as well. According to the American Society for Vascular Surgery, 17% of men and 33% of women have varicose veins.Myth #3: Varicose veins only occur with elderly people.
Although varicose veins become more common as you age, people may get varicose veins at any age.Myth #4: There are no risk factors to varicose veins. They just occur over time.
A variety of risk factors may lead to an increased risk of varicose veins including heredity, excess weight or obesity, prolonged periods of standing or sitting, pregnancy and older age. Women are also more likely than men to get varicose veins.Myth #5: Varicose veins are simply detected by seeing blue, rope-like vessels on legs or feet.
For proper diagnosis, a vascular specialist will complete a comprehensive evaluation that includes an ultrasound to detect varicose veins, evaluate blood flow and determine the efficiency of vein valves.Myth #6: There is nothing that will alleviate pain caused by varicose veins.
Small, habits or lifestyle changes may help to reduce the pain caused by varicose veins:- In order to decrease the pressure in the veins, elevate legs to the level of the heart for 30-minute increments, 4 times a day.
- People carrying extra weight may benefit from losing some weight.
- Keeping your blood circulating with regular exercise or physical activity may alleviate some pain.
- Wearing compression stockings will help to keep blood from pooling.
- Reducing salt intake since a high salt diet may lead to hypertension or narrowing of arteries.
Myth #7: Surgery is the only option to permanently treat varicose veins.
While surgery used to be the only option, there are now a range of options including quick, minimally invasive, outpatient procedures.- Vein Ablation:
- This minimally invasive technology uses ultrasound guidance to position a catheter through a small opening in the skin. Using radiofrequency, the vein is heated causing veins to close so blood is re-routed to other healthy veins. This outpatient procedure results in minimal to no scarring, bruising or swelling and patients can typically resume normal activities within a few days.
- Sclerotherapy:
- Sclerotherapy is an outpatient procedure used to treat varicose and spider veins. A tiny needle injects a solution directly into the vein to damage the lining of the vessel so it is absorbed into the body. Patients may feel a mild discomfort during the procedure. Depending on size and location of the veins, patients will respond to treatment in 3 to 6 weeks or 3 to 4 months for larger veins. Multiple sessions may be required.
- Phlebectomy:
- An outpatient procedure to surgically remove varicose veins using tiny incisions. Minimal scarring and discomfort are experienced.
Myth #8: Working on hard surfaces leads to varicose veins.
Working on hard surfaces, such as cement, does not lead to varicose veins but may contribute to musculoskeletal problems.Myth #9: Sitting for long periods of time causes varicose veins.
While is it true that venous pressure does increase with little to not activity, such as standing or sitting for long periods of time, it does not necessarily lead to varicose veins. Taking short walks, stretching or doing calf pump exercises may help to alleviate some pain and symptoms.Myth #10: If you cross your legs, you’ll get varicose veins.
This popular myth has been passed down through generations but fortunately has no merit. Varicose veins occur as a result of damaged or weakened veins. Crossing your legs does not lead to damaged or weakened veins.Myth #11: Spider veins and varicose veins are the same. Both are merely cosmetic.
Spider veins, or Telangietasias, are small, dilated capillary veins that are bluish-red in color and often appear in weblike patterns typically on legs or around the nose and lips. Spider veins are typically more cosmetic than symptomatic.Varicose veins are common and often present as rope-like blue vessels typically in the legs or feet. Varicose veins are oftentimes painful presenting with symptoms such as heaviness/fatigue in legs, leg swelling, restless leg syndrome, leg cramping while sleeping, pain, itching and burning. If left untreated, varicose veins may results in leg swelling, skin changes or venous ulcers in more severe cases.
Myth #12: Treating varicose veins is expensive and painful.
Varicose veins are oftentimes covered by insurance whereas spider veins typically are not since they tend to be cosmetic only. Patients may feel a very mild discomfort during the treatment and downtime is usually minimal afterwards depending on the size and severity of your veins.Myth #13: Varicose Veins always come back even after treatment.
This may have been true years ago but with today’s technology and treatment options, this is no longer the case. Vein ablation, Sclerotherapy and Phlebectomy are all effective treatment options and typically few patients require follow up treatments on the same veins.Myth #14: Exercise is bad for varicose veins.
To the contrary, exercise is great for varicose veins as it gets your heart pumping and your blood moving. Please note, limited exercise and compression socks may be recommended right after a varicose veins treatment to ensure blood does not pool in the legs.Myth #15: Pregnancy causes varicose veins.
Although pregnancy does not cause varicose veins it can exacerbate them. Typically harmless, varicose veins may occur when the uterus applies pressure to the large vein (inferior vena cava) which transports blood back to the heart from your lower extremities (feet or legs). Oftentimes, varicose veins will fade after delivery.Myth #16: Varicose veins are hereditary.
Varicose veins run in the family for only 50% of all people who have them. So, if your parents and grandparents had them, your likelihood is higher but it does not guarantee that you will have them. Other risk factors such as age, excess weight, prolonged sitting/standing, pregnancy and gender may increase your likelihood as well.Myth #17: Massages can cure varicose veins.
While massaging your achy legs or feet may provide temporary relief of swelling or discomfort, it does not make varicose veins go away. Advanced treatment options such as vein ablation, sclerotherapy and phlebectomy are all proven, effective treatment options.Myth #18: Compression stockings are not required/recommended before or after treatment.
Most insurance companies require patients to wear compression stockings before treatment. Compression stockings are oftentimes required post treatment, sometimes up to six weeks.Myth #19: Woman should wait until they are done bearing children to seek treatment for varicose veins.
There is no medical reason to wait until after women are done bearing children to treat varicose veins. In fact, women may benefit from having varicose veins treated before even becoming pregnant. However, if your varicose veins are treated before pregnancy, they are more likely to recur.Myth #20: Tattoos negatively affect varicose veins.
There is actually no correlation between tattoos and varicose veins.If you have questions or concerns about varicose veins or your lifestyle is being negatively impacted by the pain and discomfort of varicose veins, talk to your doctor today. A primary care physician can recommend you to a vascular specialist that can quickly and easily treat your varicose veins today.
If you’d like more information about varicose veins, please refer to your FAQ or watch our video. Feel free to reach out to us if you’d like to speak directly to a vascular specialist.